A Dynamic Duo: How CRISPR is revolutionizing CAR T Cell therapy
- Bruins for Business Health at UCLA
- Apr 23, 2024
- 4 min read
Leilani Pradis

CAR T-Cell Therapy
The immune system fights thousands of diseases every day by locating antigens,
which are proteins that elicit an immune response. These could be viruses, harmful
bacteria, and even cancer cells. However, some immune cells do not possess the right
receptors to attach to the cancer cells, preventing the immune system from demolishing
them [1].
Officially approved by the FDA in 2017, a team of researchers in the Perelman
School of Medicine at the University of Pennsylvania produced the first treatment that
harnesses the power of the immune system in defeating cancerous cells, called CAR
T-cell therapy.
CAR (chimeric antigen receptor) T-cell therapy is a type of treatment that utilizes
a patient's own immune system to fight cancer. Specifically, an individual’s T-lymphocyte
cells, which are a type of white blood cell, are manipulated in a way that causes them to bind to and destroy cancer cells. The T cells are collected and taken to a laboratory,
where a chimeric antigen receptor gene is inserted into them. These immune cells are
placed back into the patient, where they will bind to the specific antigen of the cancer
cell and hopefully kill them [2].
Currently, this immunotherapy is primarily used to battle hematologic (blood)
cancers and has had promising results. Due to the recent discovery and approval to use
CAR T-cell therapy, there are very few patients to study the long-term effects. However,
it is worth mentioning that two patients participated in a clinical trial years ago (achieving
remission in 2010), with the results being keeping their chronic lymphocytic leukemia in
remission for more than a decade [3]. This feat has further raised hopes about the
effectiveness of the treatment.
Nonetheless, there are still many limitations. Shortly, I will go over some major
limitations that can be addressed by CRISPR/Cas9 technology.
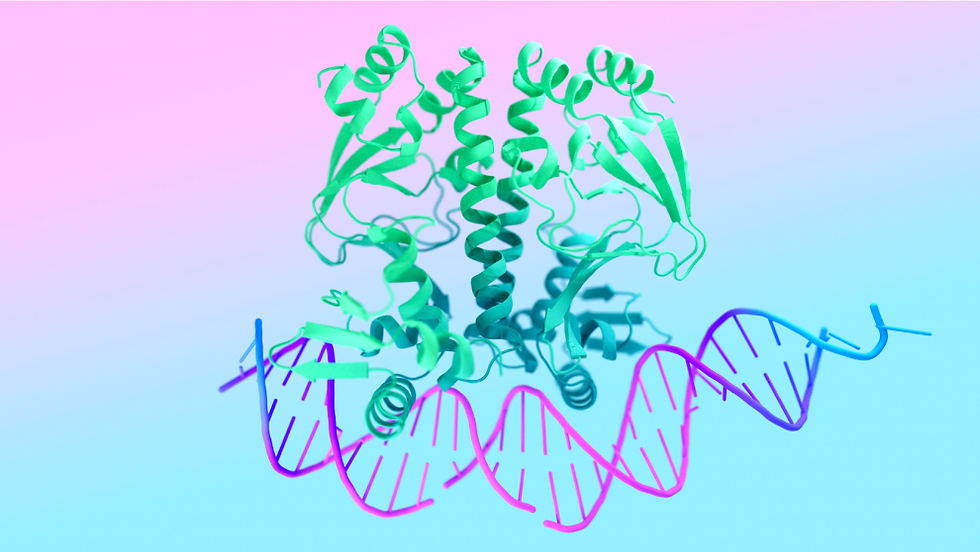
CRISPR/Cas9
CRISPR/Cas 9 is a breakthrough gene-editing tool that could be the key to
relieving many genetic diseases. CRISPR is an acronym for “clustered regularly
interspaced palindromic repeats”, which are repeating sequences in prokaryotic DNA
that serve a purpose in the organism's defense system. Cas9 stands for “CRISPR-associated protein 9”, which is an endonuclease that will make a cut on both strands in the target DNA. Briefly, this is how it works: there is a guide RNA that directs Cas9 to the target location on the DNA that will be cut. This cut allows the DNA to then be manipulated, commonly through what is called homology-directed repair. This type of repair uses a similar piece of DNA that includes any desired edits and is incorporated into the original DNA [4]. Two women made significant contributions to developing this mechanism, Jennifer Doudna and Emmanuelle Charpentier, for which they were awarded the 2020 Nobel Prize in Chemistry.
CRISPR/Cas9 is exciting because there are many things it can do, with one of its
applications to be used in a general lab setting, where it can efficiently create
animal/cell models that can be used for research like never before. Another use is
through plant science, where genetic modifications have increased bacterial resistance and even increased yield and nutrition in crops. In animal science, the tool has been
used to increase health elements in products produced by animals, such as milk, and in
research regarding pig xenotransplantation. Lastly and most relevant to this article is its
use in human science and medicine. The pair can help treat HIV, sickle cell anemia, and
even certain cancers directly [5].
Despite its vast potential, the genetic editing technology is not free from ethical
issues and debates surrounding its use. There is a great concern about the “disruption
of ecological balance” when pertaining to the use on animals, plants, and bacteria [5]. It
becomes more complicated with humans, with points bringing up legislation, safety, and
eugenics, to name a few.
How CRISPR/Cas9 can optimize CAR T-Cell Therapy
One of the major limitations of CAR T-cell therapy is cell exhaustion. This is a
state where the T-cell is no longer working efficiently, which in this case is caused by
persistent antigen stimulation. Specifically, the T-cell will not fight the cancer cells as
well (as it will have decreased cytotoxicity- that is a lower ability to be ‘toxic’ towards the
cancer cells) and tend to express proteins such as PD-1 (programmed cell death protein
1), amongst other inhibitory receptors [6]. Utilizing CRISPR/Cas9 to disrupt PD-1 has
been shown to be a possible key to reducing T-cell exhaustion. I have found two articles
where this method has been applied to two different cancers: breast cancer and
glioblastoma. In triple-negative breast cancer, there is a protein called mesothelin that is
overexpressed, which is the target for CAR T-cells. When researchers used
CRISPR/Cas9 to disrupt PD-1, they found that there was a significant increase in
cytotoxicity and cytokine production, less relapse, and greater control of the tumor [7].
With glioblastoma, a similar method was used and resulted in a decrease in t-cell
exhaustion [6]. With that said, using this gene editing tool can prove useful for
overcoming inhibiting mechanisms in CAR T-cells, making treatment more effective,
especially in solid tumors. Further, highly specific CAR T-cell therapy can take time to
develop, within that time allowing the cancer to progress. These methods have shown
promise in creating a more universal treatment, eliminating the impediment previously
stated. Cytokine secretion is an important aspect of effectual treatment using CAR
T-cells. However, one big issue with the therapy is complications such as cytokine
release syndrome, caused by the increase in cytokine excretion from immune cells.
Most cases are mild, but it can be life-threatening. Researchers have been able to
modify genes that control cytokine secretion in CAR T-cells to take out harmful/toxic
secretion while amplifying the ones that increase tumor-fighting abilities [8]. That is, it
has been found that certain cytokines are more beneficial in attacking cancer cells
(IL-18, IL-15 & IL-23) and increasing persistence [6]. These are possible avenues for
CRISPR/Cas9 technology to target to improve the immunotherapy.
Overall, CAR T-Cell Therapy is a novel approach to targeting cancer cells
through the immune system and continues to develop rapidly. Using other breakthrough
biotechnology tools such as CRISPR/Cas9 has been shown to make this treatment
even more effective, and new research resumes to address limitations.


Comments